Introduction
Wrist fractures are common injuries that can lead to prolonged stiffness and discomfort, impacting daily activities. This guide offers essential recovery tips and exercises to help restore movement, strength, and flexibility in the wrist. At Sahasra Physio Rehab, our focus is on holistic recovery that encourages safe, effective healing with lasting results.
The wrist
joint (also known as the radiocarpal joint) is a synovial joint in the upper limb, marking the area of transition between the forearm and the hand. The wrist joint is formed distally by the proximal row of carpal bones (except the pisiform); Scaphoid ,lunate and triquete.
The wrist joint is formed proximally by the distal end of the radius and the articular disc.Multiplanar wrist motion is based on three articulations: Radio scaphoid, Radio lunate distal radioulnar joint
The ulna is not part of the wrist joint – it articulates with the radius in two locations, the superior and the inferior radio-ulnar joint. Eighty percent of axial load is supported by the distal radius and twenty percent by the ulna. A fibro cartilaginous disc, called the articular disc, lies over the superior surface of the ulnar.
This disc prevents the ulnar from articulating with the carpal bones. Together, the carpal bones form a convex surface which articulates with the concave surface of the radius and articular disc.
There are several known ligamentous attachments to the distal radius. These often remain intact during distal radius fractures. The volar ligaments are stronger and give more stability to the radiocarpal articulation than the dorsal ligaments.
Epidemiology /Etiology
Distal radial fractures are one of the most common fractures of the upper extremity in adults, accounting for a sixth of all fractures in the emergency department. It is seen predominantly in the older Caucasian population. There is typically a history of a fall or similar trauma to the upper extremity. Pain and swelling in the forearm or wrist are common. Bruising and deformity in the wrist or forearm are also possible.
In women, the incidence of distal radial fracture increases with age from 40 years. Before 40 years, the incidence of distal radial fracture is much higher in men. Distal radial fractures in younger adults are usually the result of a high-energy trauma such as a motor vehicle accident, fall from height or athletic participation. In older adults, they are often the result of a low-energy or moderate trauma such as falling from standing height. This may reflect the greater fragility of the bone due to osteoporosis in the older adult.
Characteristics/Clinical Presentation
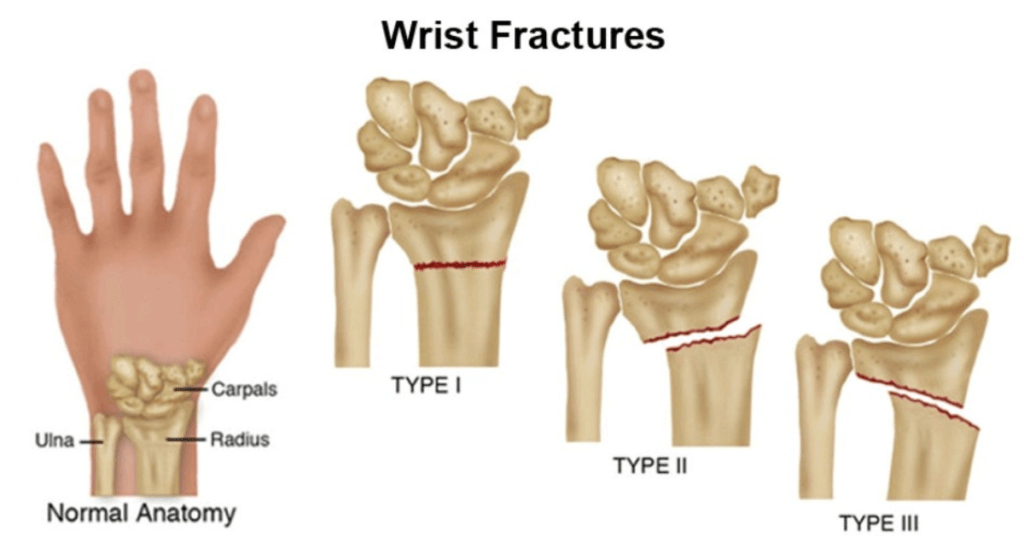
Distal radial fractures can be classified based on their clinical appearance and typical deformity. Dorsal displacement, dorsal angulation, dorsal comminution and radial shortening may all be used to describe the presentation of the fracture. Classification based on fracture patterns such as intra-articular (articular surfaces disrupted) or extra-articular (articular surface of radius intact) may also be used.
1. Classification of intra-articular fracture
- Type Ι: stable, without comminution
- Type ΙΙ: unstable die-punch, dorsal or volar; a: reducible, b: irreducible
- Type ΙΙΙ: spike fracture; contuses volar structures
- Type ΙV: split fracture; medial complex fractured with dorsal and volar fragments displaced separately
- Type V: explosion fracture; severe communication with major soft-tissue injury
2. Classification of extra-articular fracture
- Type A: extra-articular
- Type A1: extra-articular ulna, radius intact
- Type A2: extra-articular radius, ulna intact
- Type A3: extra-articular, multi fragmentary radius fracture
Types of Fractures
1.Colles Fracture
Colles fracture is typically seen as a result of a fall on an outstretched hand and results in a dorsal extra-articular or intra-articular displacement of the fractured radius:
- Intra-articular fractures are generally seen in the younger age group secondary to higher energy forces
- More than 90% of distal radius fractures are Colles’ fractures
2.Smith’s Fracture
This is a reverse Colles’ with a volar displacement, resulting from a fall on a flexed wrist with forearm fixed in supination
3.Barton’s Fracture
This is an intra-articular fracture with subluxation or dislocation of the carpus bone.
Complications
They may be the result of injury or treatment and are associated with poorer outcomes. These can include:
- upper extremity stiffness
- carpal tunnel syndrome or medial nerve involvement
- malunion
- carpal instability
- DRUJ dysfunction
- Dupuytren’s disease
- radiocarpal arthritis
- tendon/ligament injuries
- post-traumatic osteoarthritis
- compartment syndrome
- infection (mostly by open fractures)
- complex regional pain syndrome
Differential Diagnosis
Because the mechanism of injury for a distal radial fracture is usually a high energy traumatic incident, radiographs should be taken to confirm the diagnosis and ensure that the surrounding tissues are still intact. Other injuries causing radial sided pain may include TFCC tear or perforation, Galeazzi fracture (fracture to the distal 2/3 of the radius), scaphoid fracture, or radiocarpal ligament injury.
- Malunion – Distal radius malunion is the most common complication, affecting up to 17% of patients. Physical therapists may assess the effect of malunion to determine if surgery is appropriate by performing a detailed physical exam that includes a preoperative history, location and severity of pain, and functional loss
- Compartment Syndrome – This complication affects only 1% of patients. Elevate, observe, and loosen cast immediately if compartment syndrome is suspected
- Complex Regional Pain Syndrome (CRPS)- This complication is observed in 8-35% of patients. CRPS should be suspected when pain, limitations in ROM and swelling are disproportionate to the injury. There may also be changes in skin temperature and sweating. In order to obtain a good functional outcome for this patient population, early recognition and a multidisciplinary treatment approach are essential. This approach should include psychiatric and physical/occupational therapy interventions to address pain and functional limitations.
- Dupuytren’s Disease – Patients develop mild contractures in the palm along the fourth and fifth rays within six months of a distal radial fracture. The severity of the contractures determines the treatment course
- Nerve Pathology – Neuropathy may present acutely or throughout treatment. The median nerve is most common (4%), however 1% of patients have ulnar or radial involvement.
- Acute Carpal Tunnel Syndrome – Physiotherapists must be able to identify acute carpal tunnel syndrome, as delayed treatment is associated with poor outcomes, incomplete recovery or a prolonged functional recovery time
- Tendon Complications – Physiotherapists should be prepared to refer patients to surgery in the event of tendon complications secondary to irritation with inflammation or rupture from impingement.
- Capsule Contracture – Even after physical therapy treatment, some patients do not regain full forearm rotation due to contracture of the distal radioulnar joint capsule. Dorsal contracture limits pronation, volar contracture limits supination, and both may occur together. A DRUJ capsulectomy may be considered if functional ROM is not regained.
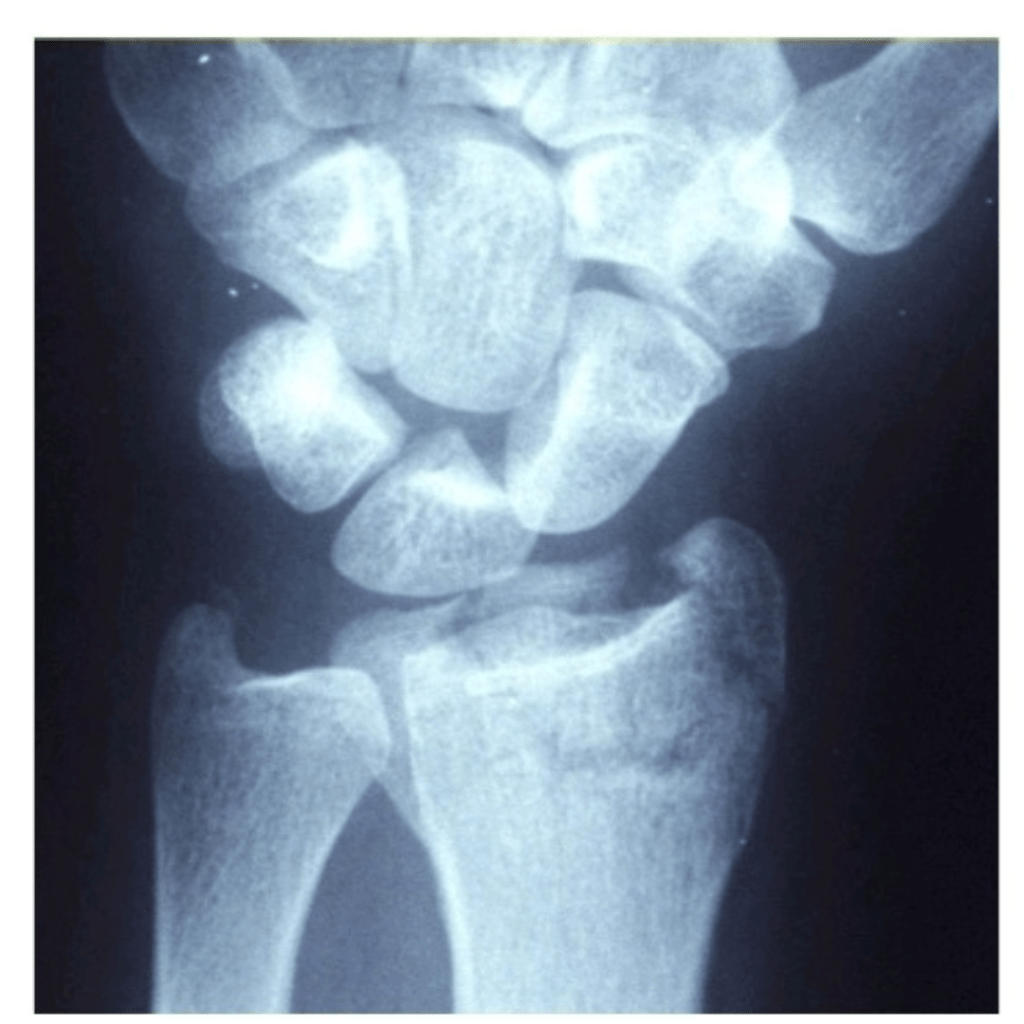
Diagnostic Procedures
Radiographic parameters are used to check detect anatomical anomalies. Classification systems should follow the following two principles:
- The classification should prescribe the treatment
- The classification should suggest the long-term, functional results of treatment or be correlated with these anticipated results
Outcome Measures
A Wrist Fracture Complication Checklist and Score Sheet was developed to improve prospective data collection The checklist includes a classification for all DRF complications, each of which is graded for severity (Mild = 1, Moderate = 2, Severe = 3). A total score is then calculated. The categories of the questionnaire are
- nerve complications
- bone/joint complications
- tendon complications
Self-Report Outcome Measures
- Visual Analogue Scale (VAS) to evaluate pain
- The Disability of the Arm, Shoulder and Hand questionnaire (DASH)
- The Patient-Rated Wrist Evaluation (PRWE)
- The Michigan Hand Outcomes Questionnaire (MHQ) is a hand-specific outcome instrument divided in six scales:
- overall hand function
- activities of daily living
- pain
- work performance
- aesthetics
- patient satisfaction with hand function
Physical Outcome Measures
- ROM of the wrist with a goniometer
- Grip Strength is an important outcome measure because it is an important function in daily activities, it can be measured with a dynamometer, Hand-held dynamometer or Jamar hydraulic hand dynamometer can be used.
Examination
Physical therapists must conduct a thorough physical exam including subjective and objective information.
- Subjective exam includes any information given by the patient such as pain experienced, limitations of ROM of the wrist and activity limitations.
- Objective exam includes assessment of wrist and digit ROM, grip and forearm strength, bony and soft-tissue abnormalities, skin integrity and nerve involvement. Be aware that the contralateral extremity may be an unreliable control.
Health care professionals should evaluate the ligamentous integrity in the presence of persistent pain associated with suspected carpal instability as early as possible in order to avoid poor functional outcomes and prolonged recovery. Specific fracture patterns and high energy injuries are strongly indicative of intercarpal ligament involvement.
To confirm the diagnosis, x-rays can identify fracture, displacement as well as the number of bony fragments.
Medical Management
Non-surgical Treatment
When the fracture is in an acceptable position, a plaster cast can be applied until the bone heals. If the fracture is displaced, the fragments are realigned (reduced), after which a splint or cast is applied. The cast will be changed two to three weeks after application as the swelling decreases and then removed six weeks after the reduction, assuming an acceptable level of healing has occurred. After this, physical therapy can start to improve the function of the injured wrist.
Surgical Treatment
If the displaced of the fracture is large enough that reduction is insufficient to achieve acceptable position of the bones, surgery is required.
Orthopedic surgeons typically recommend surgical repair of displaced articular fractures of the distal radius for active, healthy people. The sheer variety of reduction and fixation options is clear given the publication of a series of five Cochrane reviews focusing on this topic alone. Methods include: 1) closed reduction and percutaneous pinning, either extra-focal or intra-focal, 2) bridging external fixation with or without supplemental Kirschner-wire fixation, 3) dorsal plating, 4) fragment-specific fixation, 5) open reduction and internal fixation with a volar plate through a classic Henry approach, 6) a combination of these methods. According to Bushnell and Bynum (2007), surgical “complications include edema, hematoma, stiffness, infection, neurovascular injury, loss of fixation, recurrent malunion, nonunion or delayed union, instability, tendon irritation or ruptures, osteoarthritis, residual ulnar-side pain, median neuropathy, complex regional pain syndrome, and problems with the bone-graft harvest site.”
Radiographic image of external fixator
- External Fixation – External fixation is typically a closed, minimally invasive method in which metal pins or screws are driven into the bone via small incisions in the skin. These pins can then be fixed externally by either a plaster cast or secured into an external fixator frame. In comparison to a standard immobilization procedure, external fixation of distal radius fractures reduces redisplacement and yields better anatomical results. However, current evidence for better functional outcomes from external fixation is weak and is also associated with high risk for complications such as pin site infections and radial nerve injuries.
- Internal fixation – Internal fixation involves open surgery where the fractured bone is exposed. Dorsal, volar or T-plates with screws may be used. However, due to the invasive and demanding nature of open surgery, there is an increased risk of infection and soft-tissue damage and therefore this type of fixation is usually reserved for more severe injuries.
- Bone Grafts – Upon reduction of distal radial fractures, bony voids are common and can be reduced by inserting bone grafts or bone graft substitutes. Autogenous bone material obtained from the patient themselves or allogenous bone material obtained from cadaver or live donors can be used as filler for reducing bony voids. However, there is a risk of complications including infection, nerve injury or donor site pain, and there is limited evidence that bone scaffolding may improve anatomical or functional outcomes. Bone grafting is required by most procedures except closing wedge.
Radiographic image of internal fixator plate
- Percutaneous Pinning – Another strategy in reducing and stabilising the fractures is percutaneous pinning, which involves insertion of pins, threads or wires through the skin and into the bone] This procedure is typically less invasive and reduction of the fracture is closed upon which the pins placed in the bone are used to fix the distal radial fragment. Current indications for the best technique of pinning, the extent and duration of immobilization are uncertain, thus the risk of complications likely outweighs the therapeutic benefits of pinning.
- Closed Reduction – In closed reduction, displaced radial fragments are repositioned using different maneuver’s while the arm is in traction. Different methods include manual reduction in which two people pull in the opposite directions to produce and maintain longitudinal traction and mechanical methods of reduction including the use of “finger traps.” However, there is insufficient evidence establishing the effectiveness of different methods of closed reduction used in treating distal radial fractures.
Arthroscopic-assisted reduction
– This technique has many advantages over open reduction. In addition to being less invasive, it allows for direct visualization and reduction of articular displacement, the opportunity to diagnose and treat associated ligamentous injuries, the removal of articular cartilage debris as well as lavage of the radiocarpal joint. The primary limitations for arthroscopic reduction are due the limited number of surgeons with experience, a longer, more difficult procedure, and the potential for compartment syndrome or acute carpal tunnel syndrome with fluid extravasation.
Understanding Wrist Fracture Stiffness
After a wrist fracture, stiffness can develop due to immobilization in a cast or splint, limiting movement for a prolonged period. When the joint is not moved, it can lose flexibility and strength. This stiffness can affect the surrounding muscles and joints, often leading to discomfort and limited range of motion even after the bone has healed.
Importance of Early Intervention in Wrist Stiffness Recovery
- Minimizing Pain and Discomfort: Early intervention with appropriate exercises can help reduce pain and discomfort.
- Preventing Long-term Complications: Proper rehabilitation prevents long-term stiffness and enables smoother recovery.
- Enhancing Daily Functionality: Regaining wrist motion is essential for daily tasks like writing, lifting, and other routine activities.
At Sahasra Physio Rehab, we prioritize early intervention and gradual movement to support optimal recovery.
Essential Tips for Wrist Stiffness Recovery
- Follow Your Doctor’s Instructions: Always consult your physician or therapist before beginning any exercise routine post-fracture.
- Be Consistent with Your Exercises: Consistent movement, even if minimal, aids in preventing stiffness from worsening.
- Stay Hydrated and Maintain a Balanced Diet: Proper nutrition supports healing and muscle function.
- Manage Pain and Swelling: Use ice or prescribed medications to reduce swelling or pain, making exercises easier.
Physio Therapy Options at Sahasra Physio Rehab
Our trained physiotherapists at Sahasra Physio Rehab provide personalized wrist rehabilitation plans tailored to each patient’s needs, including:
- Cryotherapy/Heat Therapy: To reduce stiffness and increase blood flow, aiding in the healing process.
- Ultrasound Therapy: For deep-tissue healing and pain reduction.
- IFT/TENS
- Extra Corporeal Shockwave therapy
- Manual Therapy: Skilled therapists use hands-on techniques to improve joint movement and relieve stiffness.
- Stretching and Strengthening Programs: A customized plan to promote long-term mobility and strength in the wrist.
Top Exercise to Relieve Wrist Fracture Stiffness
1. Wrist Flexion and Extension
- How to Perform: Sit comfortably with your forearm resting on a table and the hand hanging over the edge. Slowly bend your wrist upward, then downward, in a controlled manner.
- Repetitions: Perform 10-15 reps, 2-3 times a day.
- Benefits: Increases range of motion and flexibility.
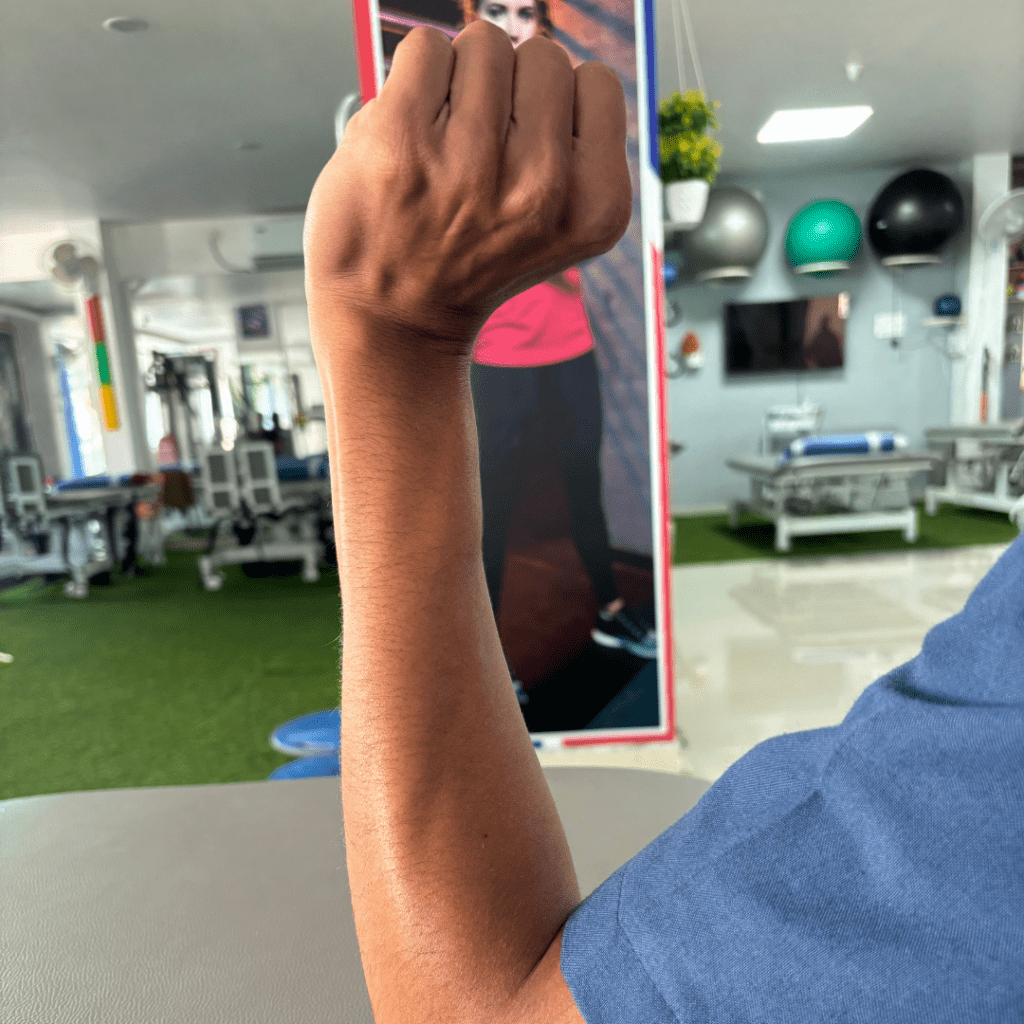

2. Wrist Rotations
- How to Perform: Hold your arm out with your elbow bent at 90 degrees. Gently rotate your wrist in clockwise and counterclockwise directions.
- Repetitions: 10 rotations in each direction.
- Benefits: Helps restore the wrist’s natural movement and prevents stiffness
- How to Perform: Use a small stress ball or therapy putty. Squeeze and hold for a few seconds, then release.
- Repetitions: Repeat 10 times, 2-3 times a day.
- Benefits: Enhances grip strength and improves muscle tone in the wrist.

4. Pronation and Supination (Palm Up and Down)
- How to Perform: With your elbow tucked into your side and arm at 90 degrees, turn your hand so the palm faces up, then down.
- Repetitions: Repeat 10 times on each side.
- Benefits: Increases rotation and reduces stiffness in wrist movement.
5. Passive Wrist Stretch
- How to Perform: Using the other hand, gently pull the fingers back towards you, stretching the wrist and forearm muscles.
- Repetitions: Hold for 10-15 seconds, and repeat 2-3 times.
- Benefits: Reduces tension in the wrist and forearm muscles, improving flexibility.
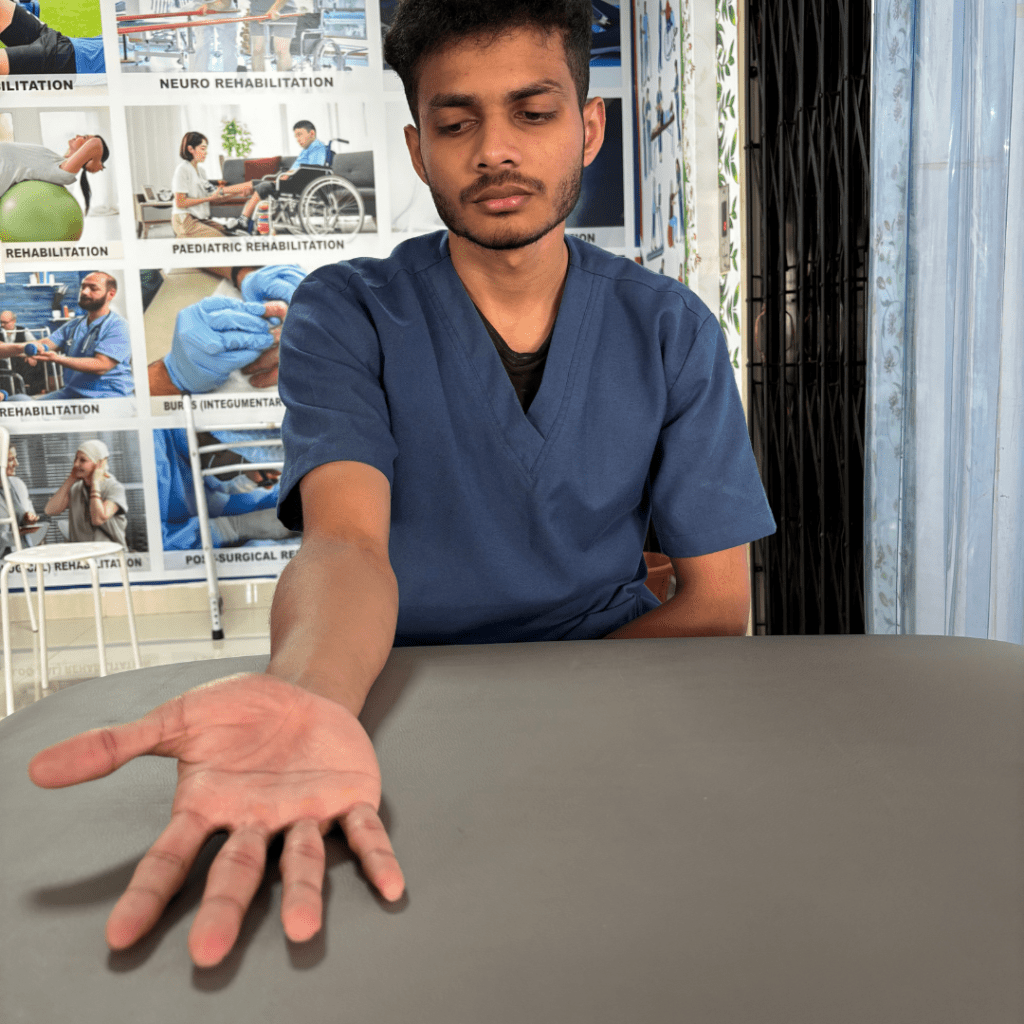
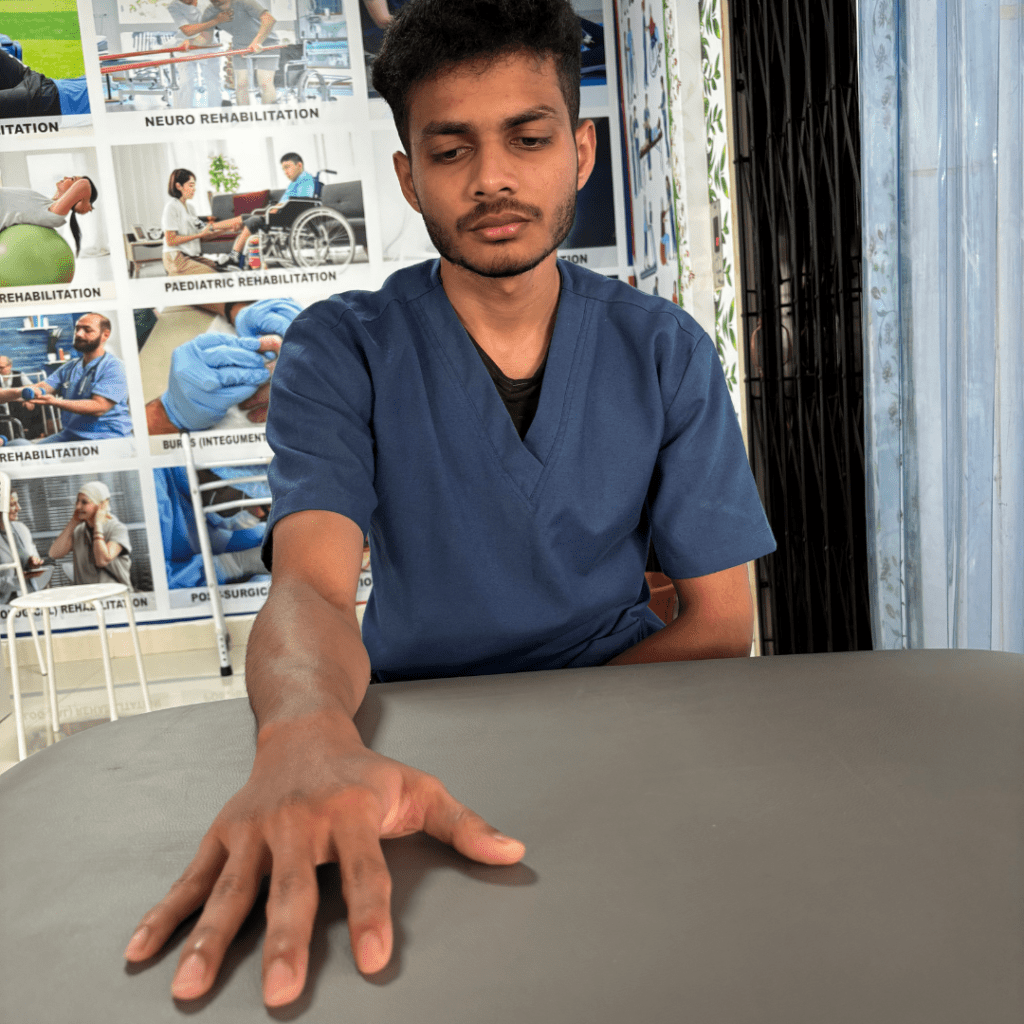
6.Ulnar & Radial Deviation
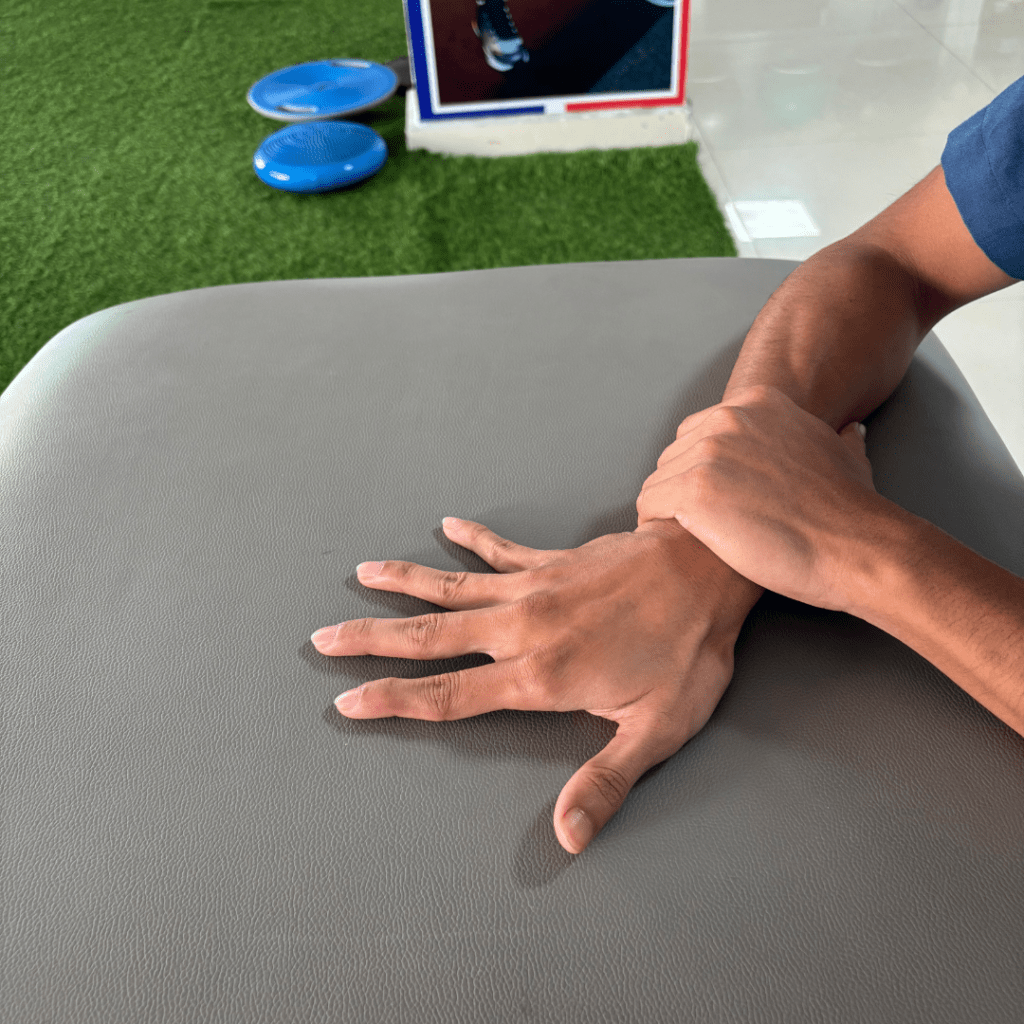
How to Perform: Put your palm flat on the table, Use the opposite hand to stabilize your forearm just above your wrist, move your wrist as much as you can from side to side, leaving your palm flat on the table at all times
Benefits: Reduces tension in the wrist and forearm muscles, improving flexibility
How to Perform: Using the other hand, gently pull the fingers back towards you, stretching the wrist and forearm muscles.
Repetitions: Hold for 10-15 seconds, and repeat 2-3 times.
When to Seek Professional Help
While self-care and exercises are essential for recovery, some cases of wrist fracture stiffness may need professional assistance. If you notice severe pain, swelling, or a lack of improvement in motion, schedule an appointment with Sahasra Physio Rehab to get a comprehensive recovery plan.
Conclusion
Recovering from a wrist fracture takes time and patience, but with the right exercises and consistent practice, you can regain flexibility and strength in your wrist. At Sahasra Physio Rehab, we’re here to support you on every step of your journey to a pain-free, mobile wrist.
For further information or personalized treatment, contact us today and let us help you restore movement and confidence in your wrist

