November 14 marks World Diabetes Day, a global campaign led by the International Diabetes Federation (IDF) and the World Health Organization (WHO) to raise awareness about diabetes, its impact, and ways to prevent and manage this condition. As diabetes rates rise worldwide, understanding and addressing its causes, symptoms, and management has become more critical than ever.
What is Diabetes?
Diabetes is a chronic health condition where the body either doesn’t produce enough insulin or cannot use insulin effectively. Insulin, a hormone produced by the pancreas, helps regulate blood sugar levels. properly managed.

The Growing Impact of Diabetes Worldwide
According to the World Health Organization (WHO), there is an estimated 422 million people with diabetes worldwide and with most of these individuals living in low and middle-income countries]. This is beside the estimated projection by the international diabetes federation that 1 in 10 persons worldwide will have T2D by 2035. It has also been reported by WHO that 1.6 million deaths can be directly linked to diabetes yearly. The aforementioned report went on to say that there is however a unified global target to prevent the rise in diabetes and obesity by 2025, Rapid urbanization, changing diets, and sedentary lifestyles contribute to the increase in diabetes cases, particularly in developing countries. This trend underlines the need for effective public health policies and awareness programs to encourage preventive measures.
The Significance of World Diabetes Day
World Diabetes Day on November 14 highlights the importance of understanding diabetes and fostering public support for those affected. The day also commemorates Dr. Frederick Banting, who, along with Dr. Charles Best, co-discovered insulin in 1921—a breakthrough in diabetes treatment.
The theme for 2024,
The theme for World Diabetes Day 2024 is “Breaking Barriers, Bridging Gaps”. This theme emphasizes the importance of:
1.Reducing the risk of diabetes
2.Ensuring that people with diabetes have access to quality care and treatment
3.Improving people’s quality of life through effective diabetes management
4. Raising awareness about diabetes everyone with affordable access to diabetes treatment, education, and support. This theme reinforces the need for governments, healthcare providers, and communities to unite in making diabetes care accessible and inclusive for all.
Types of Diabetes
The American Diabetes Association (ADA) classifies diabetes into four categories namely:
1.Type 1 Diabetes which is an absolute deficiency of insulin due to an autoimmune destruction of β cells in the pancreas. This also includes latent autoimmune diabetes of adulthood.
2.Type 2 Diabetes occurs from insulin resistance and a progressive reduction in insulin secretion. T2D is largely attributed to physical inactivity and excess body weight
3.Gestational Diabetes, which is diabetes diagnosed in the second or third trimester of pregnancy and was not present prior to the pregnancy period.
4.Specific type diabetes that are due to other causes such as monogenic diabetes syndromes, diseases of the exocrine pancreas, and drug or chemical induced.
Clinical Presentation:
• increased thirst
• increased urination,
• lack of energy and fatigue,
• bacterial and fungal infections
• delayed wound healing.
• may also complain of numbness or tingling in hands or feet or with blurred vision.
• Can have modest hyperglycemia, which can proceed to severe hyperglycemia or ketoacidosis due to infection or stress. T1DM patients can often present with ketoacidosis (DKA) coma as the first manifestation in about 30% of patients
• Persons with DM (usually Type 1) may experience weight loss because of the improper fat metabolism and breakdown of fat stores.
Diagnostic Procedures
Fasting glucose level of greater than 126 mg/dl on two separate occasions is considered positive, with fasting defined as no caloric intake for at least 8 hours preceding the test, The strictest procedure is according to the World Health Organization, which states that the diagnosis is positive if “venous plasma glucose concentration is greater than 11.1 mmol/L 2 hours after a 75g glucose tolerance test.”
Risk factors for T2D may include:
• Family History
• Obesity
• Sedentariness
• Increasing Age
• History of Gestational Diabetes
• Race (more common with African American, American Indian, Hispanics and Asian American
Complications of Diabetes
Over time, diabetes causes damage to various systems of the body including: cardiovascular, neurological, musculoskeletal and integumentary systems with increased risk of developing comorbidities. It is known to affect specific organs such as the eyes, kidneys, nerves and heart. These complications may be categorized as acute or chronic.
Acute: Hypoglycemia, Diabetic ketoacidosis & Hyperosmolar non ketotic coma
Chronic:
1. Microvascular complications consisting:
◦ Retinopathy
◦ Nephropathy
◦ Neuropathy (including peripheral distal symmetric polyneuropathy, autonomic neuropathy, proximal painful motor neuropathy and cranial mono neuropathy)
2. Macro vascular complications including:
◦ Cardiovascular disease
◦ Peripheral vascular disease
◦ Stroke
Management of Diabetes
Management can either be pharmacological or non-pharmacological. To effectively tackle diabetes and its complications, lifestyle adjustments including diet and exercise are often recommended to ensure optimal health. Also patients are encouraged and educated on how to manage their conditions by themselves to achieve optimal results from the lifestyle modifications. Diabetes treatment is mainly aimed at glycemic control, improving quality of life of patients, preventing complications and ultimately reducing mortality in this patient population.
Pharmacological Interventions
1. Insulin Therapy: This is an essential treatment in patients with type 1 diabetes as the condition is marked with a dysfunction in β cell function to achieve best results and to prevent metabolic disturbances, the administration of insulin is recommended to be through injections given on a daily basis or via a continuous subcutaneous pump.
2. Pramlintide is an adjuvant glucose lowering medication that acts based on the naturally occurring β-cell peptide, amylin and is recommended for use in patients with type 1 diabetes.
3. Metformin is the preferred medication for the management of type 2 diabetes.
4. Sulfonylureas can either be used instead of metformin if the patient is not overweight or unable to tolerate metformin and it can be administered with metformin if glycemic control is inadequate.
Non-pharmacological Interventions
The non-pharmacological management of diabetes is basically centered on lifestyle changes with exercise and diet being the main stay of the programme. Lifestyle modification is recommended to avoid infusion with insulin.
Nutritional Intake
Integrating an individualized meal plan is essential to achieving positive outcomes with these patients. The portion and types of food eaten may affect the balance of insulin and consequently, levels of blood glucose. It has been reported that the quality of the dietary intake rather than the quantity is more important. As such, diets rich in whole grain, fruits, vegetable, nuts; lower in refined grains, red or processed meat and sugar-sweetened beverages; and moderate in alcohol are recommended as they help improve glycemic control and lipids in patients with diabetes.
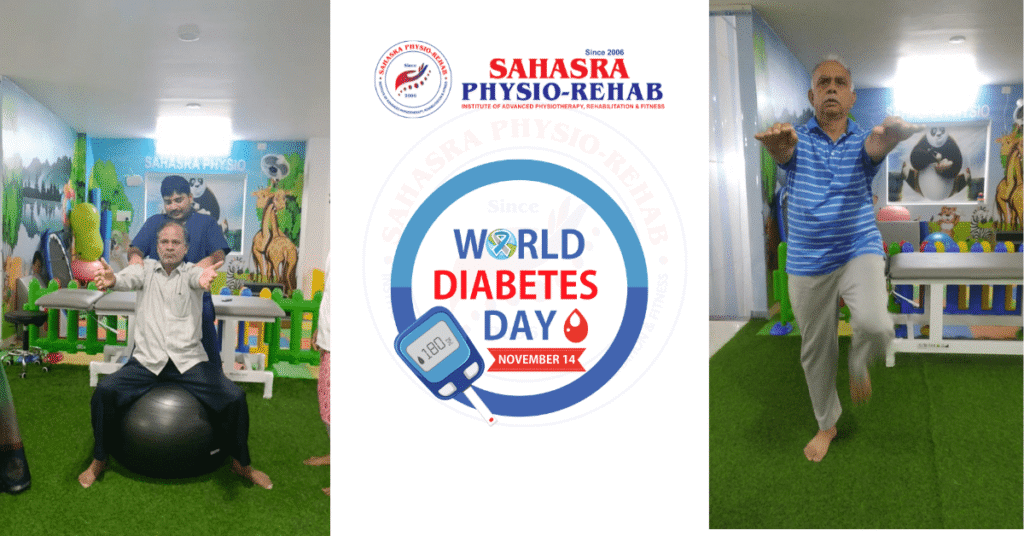
Diabetic Rehabilitation
Physical Activity & Exercise
Physical activity (PA) is any form of movement that promotes the use of energy, while exercise is any planned and/or structured PA and are both beneficial for all patients with diabetes. Exercise programmes are geared towards improving quality of movement,
participation in activities of daily living, managing pain if any, lowering blood sugar and ultimately slowing the progression of the condition and its multi systems complications.
A combination of aerobic and resistance training exercises has been recommended in planning exercise programmes for this population as it has been reported to produce positive effects on blood glucose levels. Flexibility and balance exercises are reported to be beneficial for older patients with diabetes as the former will help in improving range of motion at joints, while the latter can aid in reducing fall risks.
While exercise may be good, precautions should be taken to avoid exercise related complications in patients with diabetes for which the ADA recommends that
- There should be appropriate progression of exercises to minimize risk of injury
• People, especially older ones, with diabetic complications such as autonomic neuropathy, cardiovascular or pulmonary disease should avoid exercising outdoors on very hot and humid days.
• Doses of medications with tendency to cause hypoglycemia besides insulin should be adjusted based on exercise training.
• Exercise-induced hyperglycemia, which is more common in patients with T1D, can be mitigated with either a lower intensity aerobic cool down or insulin administration.
• Resistance exercise should be performed before aerobic exercise in the same session to prevent exercise-induced hypoglycemia
Benefits of Exercising:
Physiotherapy is an important part of diabetes management. Physiotherapist recommends exercises that cause muscles to use sugar for energy. With the help of regular exercises, the body uses insulin more efficiently. Lack of activity and being obese are the most significant environmental factors related to Type 2 diabetes. Increased activity and increasing exercise levels promote weight loss. It increases the body’s sensitivity to insulin and enhances the utilization of glucose. It helps to lower blood sugar levels and maintain overall diabetic control. Exercising regularly and losing weight are beneficial in glycemic control in Type 1 and Type 2 diabetes and also help prevent the development of diabetes in people who have prediabetes.
Exercises for Diabetic Patients:
The physiotherapist designs a structured exercise program according to the patient’s needs. Structured Exercise programs consist of resistance training and aerobic exercises. Top of Form
The 3 main types of exercise for diabetic patients are aerobic, strength, and flexibility exercises. A diabetic person should start with aerobic exercises, then slowly progress to strengthening exercises and then progress to flexibility exercises, with two sessions of strength training per week.
Walking: Brisk walk of 30 minutes, 5 days a week is recommended. It is a simple and safe exercise and just requires a good pair of shoes and a safe place to walk.
Cycling: Cycling is a low-impact exercise for lower joint pain, a good exercise for diabetes.
Swimming: Aquatic exercise like swimming helps reduce the blood sugar level, also is a low-impact exercise for diabetes and it helps to relax the whole body and is a good workout for the heart, lungs, and muscles.
Aerobic exercises: Aerobic exercises like aerobic dance can also be done as a workout.
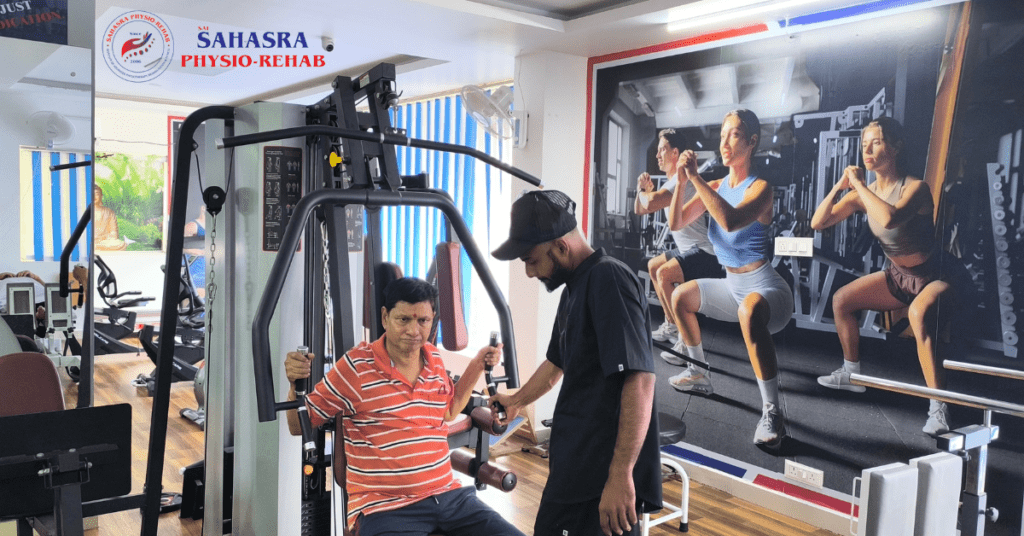
Weight training: Weight lifting and other strengthening activities help to build up muscle mass, and burn down calories. Strength training can also improve blood sugar control, thus suitable exercise for diabetes.
Resistance band exercise: Resistance band exercises can also be done by diabetic patients. With the help of simple weights or resistance bands, strengthening exercises can be done.
Calisthenics: Calisthenics is a type of strengthening exercise, where the patient’s own body weight is used to increase strength e.g. squats, pushups, pull-ups lunges, and abdominal crunches.
Pilates: Pilates is a fitness program, recommended to improve core strength, coordination, and balance.
HIIT: High-intensity interval training (HIIT) is a suitable exercise for diabetic patients. By performing High-intensity interval training, leads to rapid improvement in glucose levels in diabetic patients.
How can a Physical Therapist
Physical therapists help people with diabetes take part in safe, effective exercise programs. This can help lower your blood sugar levels. Your physical therapist can help you improve your ability to move, perform daily activities, and reduce pain. Physical therapy treatments also can help heal diabetes-related skin problems faster than without treatment.
Your physical therapist will examine your record of blood glucose levels and check your skin for wounds. They also will conduct a complete assessment of your:
• Strength.
• Flexibility.
• Endurance.
• Balance.
• Skin sensation (especially in the feet).
They will use the results of these tests to design a personalized treatment program that addresses your problems and needs. Your treatment program can help improve your:

Movement. Your physical therapist will choose specific activities and treatments to help restore normal movement. These might begin with passive movements that the physical therapist performs for you to gently move your joints. They can help you progress to active exercises and stretches that you can do yourself.
Strength. Your physical therapist can teach you the right exercises to steadily and safely restore your strength.
Flexibility. Your physical therapist will determine if any muscles are tight and help you gently stretch them. They can teach you what to do to improve your flexibility.
Endurance. Regaining your endurance is important. You may have weakness due to inactivity. Your physical therapist can teach you exercises to help you regain the energy to return to your normal activities.
Balance and coordination. Regaining your sense of balance is important to prevent falls. Coordination is also essential for daily living and work-related activities. Your physical therapist can teach you how to improve your balance and restore your coordination.
Walking ability. Your physical therapist can improve your ability to walk in comfort by adjusting your shoes or adding inserts (orthotics) to support your feet and ankles. They may teach you how to use a walker or a cane, if needed, to help you walk safely.
Pain levels. Physical therapy treatment is a safe way to treat chronic pain. Your physical therapist may use different types of treatments and technologies. They will prescribe the most effective and safe exercises for you to perform to control and reduce pain. Your physical therapist can teach you how to protect painful areas to make them less sensitive to diabetic nerve pain (neuropathy).
Blood glucose levels. Physical activity, such as prescribed exercise, can help lower your blood sugar levels. Your physical therapist can design a safe, personalized exercise program to help you control and lower your blood sugar.
Healing of sores. Your physical therapist can apply bandages, dressings, lotions, and treatments to help sores heal faster. They also may check your footwear for proper fit and overall condition. They will teach you how to perform daily foot and skin checks to prevent blisters and sores from developing.
Home exercise. Your physical therapist will teach you how to strengthen, and stretch your muscles. They also will teach you aerobic exercises to perform on your own at home. Your exercise program will be specific for your needs. Doing these exercises as prescribed can speed your recovery.
Ability to perform daily living and work activities. Your physical therapist will discuss your activity goals with you and use them to set your recovery goals. Your treatment program will help you reach your goals in the safest, fastest, and most effective way possible. Consult with a physical therapist before you begin any exercise program to address diabetes symptoms.

